
Best Treatment for Genital Warts cream (ointment, gel)
Genital Warts cream (ointment, gel) | Recommendation / Comparison / Buy / Treatment
Warts / Vulvar Condyloma Acuminatum / Genital Warts
Warts : Causes, Types, Removal, Treatment
【Causes】
What are warts?
【Types】
【Treatments include】
1.salicylic acid, duct tape,
2.cryotherapy,
3.surgery,
4.laser treatment,
5.electrocautery,
6. photodynamic therapy,
7.chemical treatments,
8.topical creams,
9.cantharidin,
10.antigen shots.
You should see your doctor if:
1.You have warts on your face or another sensitive part of your body (e.g., genitals, mouth, nostrils).
2.You notice bleeding or signs of infection, such as pus or scabbing, around a wart the wart is painful the color of the wart changes.
3.you have warts and diabetes or an immune deficiency, such as HIV/AIDS.
【Best treatments for warts 】
The best treatments for warts (vulvar condyloma acuminatum, Genital warts)
【Warts : Causes, Types, Range, Symptoms, Removal, Treatment】

【Causes】
What are warts?
1. Warts are raised bumps on your skin caused by the human papillomavirus (HPV).
2. There are more than 100 types of HPV, the virus that causes warts.
3. It can appear anywhere on the body.
4. It can look like a solid blister or a small cauliflower.
【Types / Range / Symptoms】
1.Common warts、verruca vulgaris
2.Plantar warts、verruca plana
3. Filiform warts, or verruca filiformis
4. Mosaic warts
5. Genital warts
6. Periungual wart
7. Almost all types of HPV cause relatively harmless warts that appear on your hands or feet.
8.However, there are a few strains of HPV that cause warts on, in, and around your genitals.
9. In women, these genital warts can eventually lead to cervical, anal, and vulvovaginal cancer.
10. In men, anal cancer and cancer of the glans penis can also occur as a result of infection with some types of genital warts.
11. Anyone who develops genital warts should see their doctor for assessment.
【Treatments include】
1.Salicylic acid, duct tape,
1.1 Most over-the-counter creams, gels, paints, and medicated Band-Aids contain salicylic acid.
1.2 They’ll work best if you soak the wart in water for about 10 minutes before you apply the treatment.
1.3 Do not apply salicylic acid to the face.
1.4 Because salicylic acid may destroy healthy skin.
1.5 You must use these products every day, often for a few weeks.
1.6 This approach can take several rounds of treatments to work.
1.7 If the skin becomes sore, treatment should be stopped.
2.Cryotherapy,
2.1 These over-the-counter treatments spray nitrogen onto your wart.
2.2 It destroying the cells.
2.3 A blister develops, which eventually scabs and falls off a week or so later.
2.4 This kills the skin.
2.5 This treatment must be carried out by a healthcare professional.
2.6This can be a bit painful, but usually works well.
3.Surgery,
Surgery is usually only considered if a wart hasn’t responded to other treatments.
4.Laser treatment,
Laser treatment uses a precise laser beam to destroy the wart.
5.Electrocautery,
Electrosurgery burns the wart with an electric charge through the tip of a needle.
6.Photodynamic therapy,
7.Chemical treatments,
For stubborn warts, peeling creams with glycolic acid, stronger salicylic acid, or tretinoin could do the trick.
8.Topical creams,
9.Cantharidin,
This is painless, but it creates a blister that may be uncomfortable.
10.Antigen shots.
This treatment may not be suitable during pregnancy.
Warts are often difficult to clear.
If the wart is gone but the virus remains, warts may recur.
May be difficult to eliminate completely or permanently.
You should see your doctor if:
1. You have warts on your face or another sensitive part of your body (e.g., genitals, mouth, nostrils).
2. You notice bleeding or signs of infection, such as pus or scabbing, around a wart the wart is painful the color of the wart changes.
3. you have warts and diabetes or an immune deficiency, such as HIV/AIDS.
【Best treatments for warts 】
Extract
1. The Solanum species have been used for the treatment of warts, tumor and cancer in folk medicine.
2. The S. incanum extract is an important traditional Chinese medicine in Taiwan since 1973.
3. The purpose of the present study was to evaluate the efficacy and safety of Solanum incanum (synonym: Solanum undatum) extract Solamargine, a water-soluble product primarily composed of alkaloid solamargine, for the treatment of human condyloma and to study the possible underlying anti-condyloma mechanisms.

Anti-wart pharmaceutical composition
Methods
1. We conducted a pilot study to test the effectiveness and side effects of Solamargine gel (2.3% solamargine in Solanum incanum plant extract) for the treatment of external genital warts.
2. We produced different types of human papillomavirus (HPV) E6/E7-infected cells by lentiviral technology and studied the differences in apoptosis and autophagy between these cells under the treatment of Solamargine.
Discussion
1. Patient-applied home use medications for EGW include imiquimod, polyphenon E (green tea extracts), and podofilox (a purified podophyllin), which may produce skin erosions and burning in the majority of patients.
2. The most common adverse effects of these drugs are local reactions, including erythema, pruritis/burning, pain, ulceration, and erosion, which were observed in 44% of patients using podophyllytoxin and 53.3% of patients using immiquimod [30].
3. In comparison, the Solamargine gel produces good condyloma lesion responses, much less local tissue destruction and inflammation, and has the advantage over all treatments of use at home.
4. Solamargine, which is extracted from Solanum incanum, contains alkaloid solamargine as the main active ingredient and has been show to induce cutaneous squamous cell carcinoma cell apoptosis and to inhibit tumor growth in vivo.
5. In the present study, we showed that Solamargine induced apoptosis in HPV-associated cells in vitro and induced patient condyloma regression in a clinical trial.

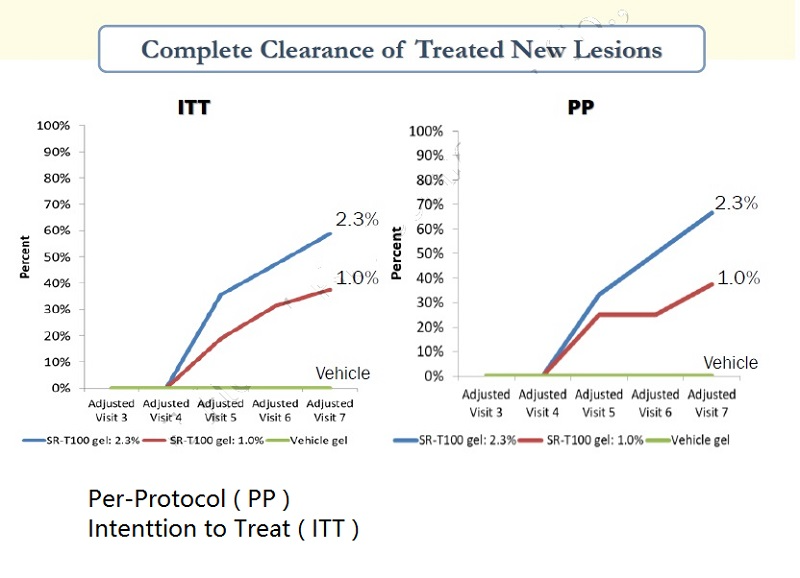

Results
1. Nineteen (73%) of 26 patients using the Solamargine gel exhibited a response, and 16 (61.5%) patients achieved total clearance.
2. Only one patient showed severe (grade 3-4) skin-related side effects.
3. Solamargine induced mitochondria-dependent apoptosis in HPV-infected cells.
4. Cells expressing the high-risk HPV E6/E7 type were resistant to Solamargine-induced apoptosis.
5. Solamargine induced a greater autophagic response in HPV 16, 18-E6/E7 cells than in HPV 6b, 11-E6/E7 cells.
6. Autophagy inhibition enhanced Solamargine-induced apoptosis in HPV 16, 18-E6/E7 cells, whereas apoptosis inhibition enhanced Solamargine-induced autophagy in HPV 6b, 11-E6/E7 cells.



 Conclusions
Conclusions
1. Solamargine is effective for the treatment of human vulva condyloma, with few side effects.
2. Compared with those with high-risk HPVs, cells with low-risk HPVs were more sensitive to Solamargine treatment.
3. Autophagy played a protective role in Solamargine-induced apoptosis in HPV-infected cells.
4. Our pilot study showed that Solamargine was effective for the treatment of human vulva condyloma and was associated with few side effects.
5. Furthermore, we showed that cells expressing LR HPVs were more sensitive to Solamargine treatment than those expressing HR HPVs.
Features :
• Prevention of UV skin damages
• Softening of skin keratinocytes
• Restores skin elastic property
• Botanically derived natural plant extraction
• No adverse skin reaction
• Patent rights protection in 32nations
• HiPreservative & Pigment free
USE: Apply several times per day, preferably covers with dermal dressing on film for the best absorption
USAGE : Patented ingredients for enhancing the repair of skin damage from environment and sunlight (as indicated in patents)
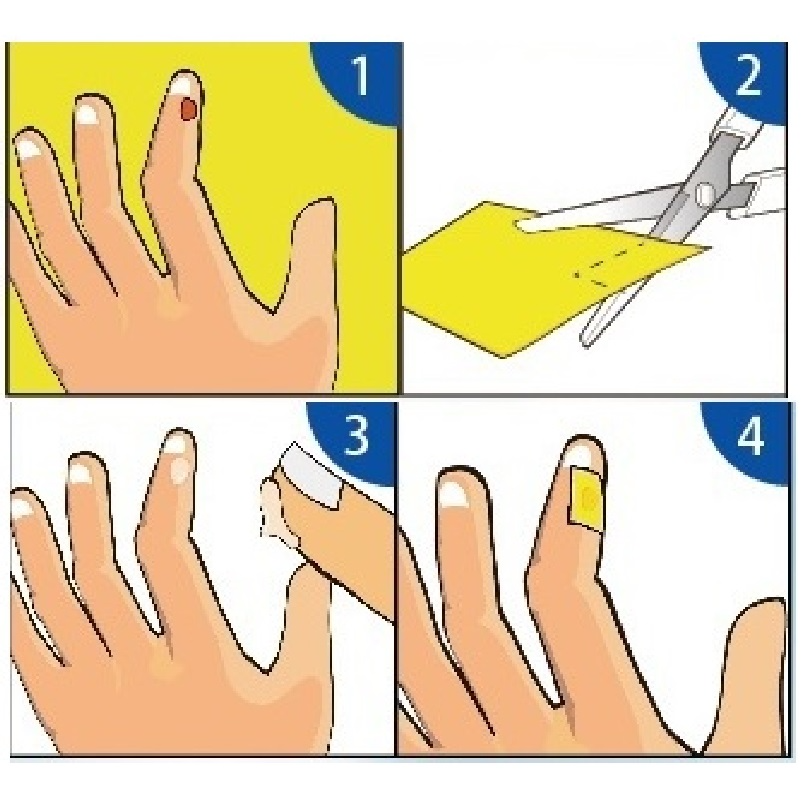 Instructions:
Instructions:
1. The cut artificial skin is large enough to completely cover the affected area.
2. Take an appropriate amount of ointment and apply it to the lesion.
3. Cover the cut artificial skin on the lesion.
TURBO Instructions:
1. In order to shorten the time course, the lesion can be treated with liquid nitrogen first, and then applied with ointment and then put a few artificial skins on the affected area.
2. If the artificial skin does not fall off, replace the ointment every two days. (Refill at any time depending on the situation)

The best treatment for actinic keratosis (Solar Keratoses / Actinic keratoses / AKs)
The best treatments for warts (vulvar condyloma acuminatum, Genital warts)
The best treatment for squamous cell carcinoma (squamous cell cancer / SCC )
The best solution for cancer cells
0 Genital Wart | Table of Contents
1 Genital Wart | Causes
2 Genital Wart | Symptoms
3 Genital Wart | Confusion | Misdiagnosis
4 Genital Wart | Contagion
5 Genital Wart | Treatment and Prevention
6 Genital Wart | See
7 Genital Wart | Reference
8 Genital Wart | External link
Genital Wart | Cause
Genital Wart are caused by human papilloma viruses (HPV).
Genital Wart is a DNA virus.
The diameter of Genital Wart virus particles is about 50-55nm.
Genital Wart mainly infect epithelial cells. Humans are the only host. Tissue culture has not been successful.
Genital Wart uses nucleic acid hybridization technology, and it is known that there are at least 28 types of HPV.
Genital Wart is clinically related to the types of HPV that cause some different types of warts.
Genital Wart | Symptoms
Genital Wart male Genital Warts patient's penis
Genital Wart patients will develop genital warts within two weeks to eight months after contact with an infected person.
Genital Wart patients may also develop eczema dermatitis in other parts of the body such as arms, head and face, neck and back, and even the belly button.
The most common symptoms in men with Genital Wart include itchy or painless flesh-colored particles on the penis, scrotum, or anus.
Female patients with Genital Warts have broccoli-like fleshy grains around the vulva or in the vagina, which are generally difficult to detect.
If the wart grows on a woman's cervix, it may cause minor bleeding.
Patients with Genital Wart will not cause serious complications.
Genital Warts women will increase the chance of developing cervical cancer.
Genital Warts data shows that 90% of cervical cancers are related to the HPV virus.
Genital Warts | Confusion | Misdiagnosis
Genital Warts is often confused with male penile pearl rash, female pseudocondyloma, etc., and some cause misdiagnosis.
Genital Warts needs to be aware that pearl rash and pseudocondyloma are harmless.
Acetic acid white test can identify whether it is Genital Warts.
Genital Warts | Contagion
Genital Warts are spread by direct contact with the exposed wounds of patients, usually through sexual intercourse.
Genital Warts indirect contact, including toilets, personal clothing, etc., can cause infection.
It is difficult for Genital Warts to eliminate pathogens through general cleaning and disinfection processes.
Condoms do not provide sufficient protection because they cannot cover all infected parts. The only safe precaution is to avoid direct contact between one's own skin and the infected tissue.
Genital Warts has very few cases showing that oral sex may cause warts in the mouth and throat.
Genital Warts | Treatment | Prevention
Genital Warts diagnostic criteria: contact history, history of non-marital sexual contact, history of spouse infection or history of indirect infection.
Genital Warts laboratory examination: skin lesion biopsy.
Genital Warts has the characteristics of histopathological changes in the characteristic hollow cells of HPV infection.
Genital Warts uses antigen or nucleic acid tests to show HPV in skin lesion biopsy when necessary.
Genital Warts is common in HPV6 and 11, and rarely in HPV16 and 18.
Genital Warts case classification: reported cases, with 1.1 and 1.2 indicators.
Genital Warts confirmed cases, with any of the indicators 1.1, 1.2 and 1.3.
Genital Warts treatment principle: pay attention to whether the patient is infected with gonococcus, chlamydia, mycoplasma, trichomoniasis, mold and other pathogens at the same time. If so, they should be treated at the same time.
If the spouse and sexual partner of Genital Warts patient have Genital Warts or other STDs, they should be treated at the same time. Avoid sex during treatment.
Genital Warts test: The test standard is to remove hyperplastic warts.
Genital Warts prognosis: Generally good, but Genital Warts has a higher recurrence rate.
Genital Warts management and prevention: Genital Warts should only be reported once per patient.
Genital Warts patients who have not been diagnosed in the past should be reported when they are first diagnosed.
Genital Warts patients should avoid sex or use condoms to prevent transmission to their spouses.
Patients with Genital Warts should be treated early.
#Peeling Products #Cryosurgery #Nitrogen #warts #Common warts #Plantar warts #Flat warts #Filiform warts #Periungual warts #Diabetes #Genitals #Freezing #reatments #salicylic acid #treatments #Surgery #Genital warts #Cervical cancer #Anal cancer #vulvovaginal cancer #genital warts #Glans penile #Contagious #HPV #hrHPV #sexual partners #vaginal #oral #anal #sex #anal cancer #anti wart


