The Best Treatment for Actinic keratosis cream (ointment, gel)
Actinic keratosis cream (ointment, gel) recommendation (comparison, where to buy)
Actinic keratosis | Causes / Range / Symptoms / Types / Prevention / treatment
【Causes】
What is actinic keratosis (AK)?
【Range / Symptoms / Types】
What are the clinical features of actinic keratosis (AK)?
【Prevention】
【Treatment Comparison】
【The best treatment for actinic keratosis (AK) 】
Solamargine(SR-T100) is best treatment for actinic keratosis (AK)
Best Treatment for Actinic keratosis cream (ointment, gel) | Actinic keratosis cream (ointment, gel) recommendation (comparison, where to buy) | Causes / Range / Symptoms / Types / Prevention / treatment

【Causes】
What is actinic keratosis (AK)?
1. AK result from long-term exposure to ultraviolet (UV) radiation.
2. Actinic keratoses are a reflection of abnormal skin cell development due to DNA damage by short wavelength UVB.
3. They are more likely to appear if the immune function is poor, due to ageing, recent sun exposure, predisposing disease or certain drugs.
4. Actinic keratosis (AK) are also known as solar keratosis.
5. If treated early, almost all actinic keratoses can be cleared up or removed before they develop into skin cancer.
6. Actinic keratosis (AK) are considered precancerous or an early form of cutaneous squamous cell carcinoma (a keratinocyte cancer).
7. Untreated lesions have up to a 20% risk of progression to squamous cell carcinoma, so treatment by a dermatologist is recommended.
【Range / Symptoms / Types】
What are the clinical features of actinic keratosis (AK)?
1. Actinic keratosis (AK) may be solitary but there are often multiple keratoses. The appearance varies.
2. It's most commonly found on your face, lips, ears, back of your hands, forearms, scalp or neck.
3. Actinic keratosis (AK) enlarges slowly and usually causes no signs or symptoms other than a patch or small spot on your skin.
4. These patches take years to develop, usually first appearing in people over 40.
5. Actinic keratoses (AK) most commonly present as a white, scaly plaque of variable thickness with surrounding redness.
6. Rough, dry or scaly patch of skin, usually less than 1 inch (2.5 centimeters) in diameter.
7. Flat to slightly raised patch or bump on the top layer of skin In some cases, a hard, wartlike surface Color as varied as pink, red or brown
8. Itching or burning in the affected area
9. The presence of ulceration, nodularity, or bleeding should raise concern for malignancy.
10. The lesions are usually asymptomatic, but can be tender, itch, bleed, or produce a stinging or burning sensation.
11. Tender, thickened, ulcerated or enlarging actinic keratoses should be treated aggressively.
【Prevention】
1. Limiting extent of sun exposure
1.1 Avoid sun exposure during noontime hours between 10:00 AM and 2:00 PM when UV light is most powerful.
1.2 And avoid staying in the sun so long that you get a sunburn or a suntan.
1.3 Minimize all time in the sun, since UV exposure occurs even in the winter and on cloudy days.
2 Using sun protection
Wearing sun protective clothing such as hats, sunglasses, long-sleeved shirts, long skirts, or trousers
【Treatment Comparison】
Treatment
There are a variety of treatment options for AK depending on the patient and the clinical characteristics of the lesion.
Although overall cure rates are high, experts agree that the best treatment for AK is prevention.
1. Physical treatments
Physical treatments are used to destroy individual keratoses that are generally symptomatic or have a thick hard surface scale.
1.1 Cryotherapy using liquid nitrogen
1.2 Shave, curettage and electrocautery
a. Shave, curettage (scraping with a sharp instrument) and electrocautery (burning) may be necessary to remove a cutaneous horn or hypertrophic actinic keratosis (AK).
b. Healing of the wound takes several weeks or longer, depending on the body site.
1.3 Excision
a. Excision ensures the actinic keratosis (AK) has been completely removed, which should be confirmed by pathology.
b. The surgical wound is sutured (stitched). The sutures are removed after a few days, the time depending on the size and location of the lesion.
c. The procedure leaves a permanent scar.
2. Medication / Field treatments / Creams
2.1 Topical medications are often recommended for areas where multiple or ill-defined AK are present, as the medication can easily be used to treat a relatively large area.
2.2 Creams are used to treat areas of sun damage and flat actinic keratoses, sometimes after physical treatments have been carried out.
2.3 Field treatments are most effective on facial skin.
2.4 Creams are pretreatment with keratolytics (such as urea cream, salicylic acid ointment or topical retinoid), and thorough skin cleansing improves response rates.
2.5 The course of treatment may need repeating from time to time.
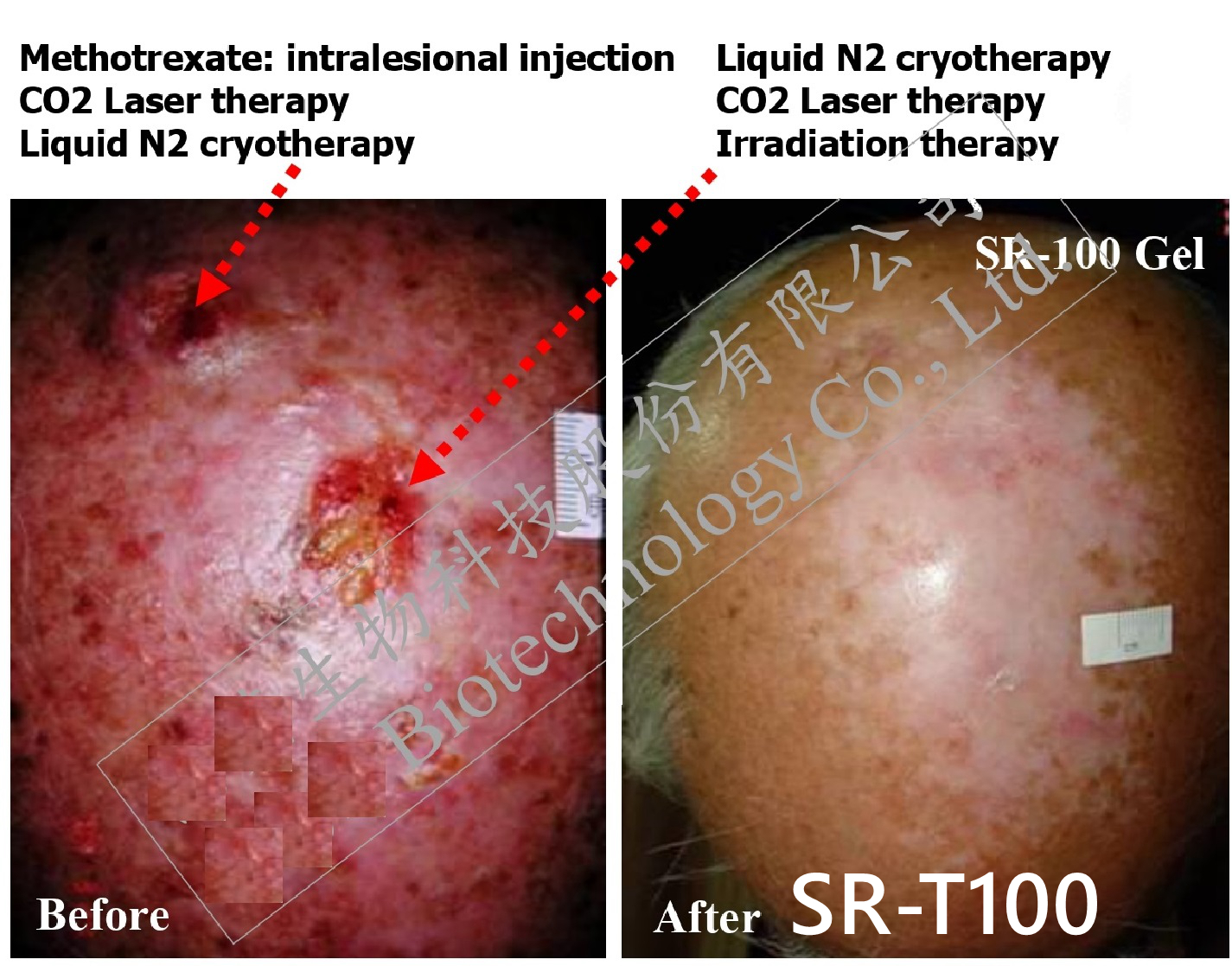
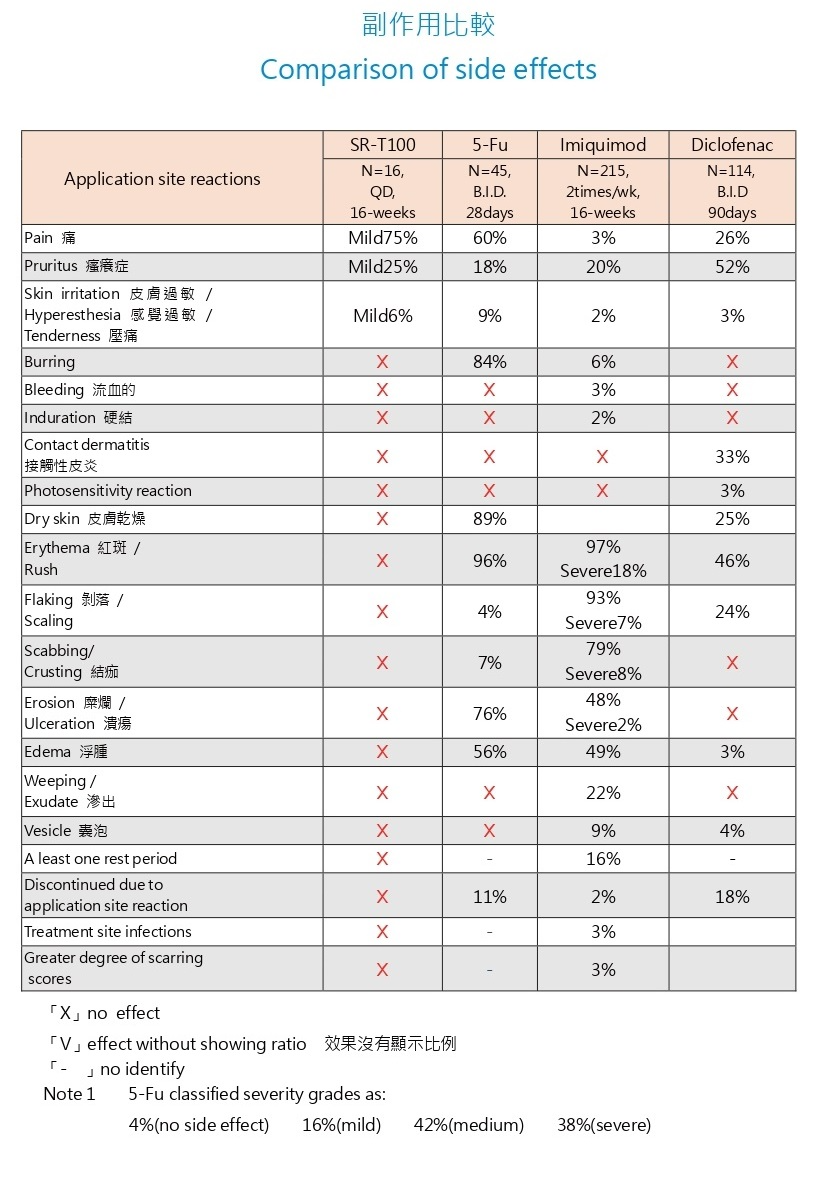
2.6 With the exception of Solamargine(SR-T100) gel, field treatments all result in local inflammatory reactions such as redness, blistering and discomfort for a varying length of time.
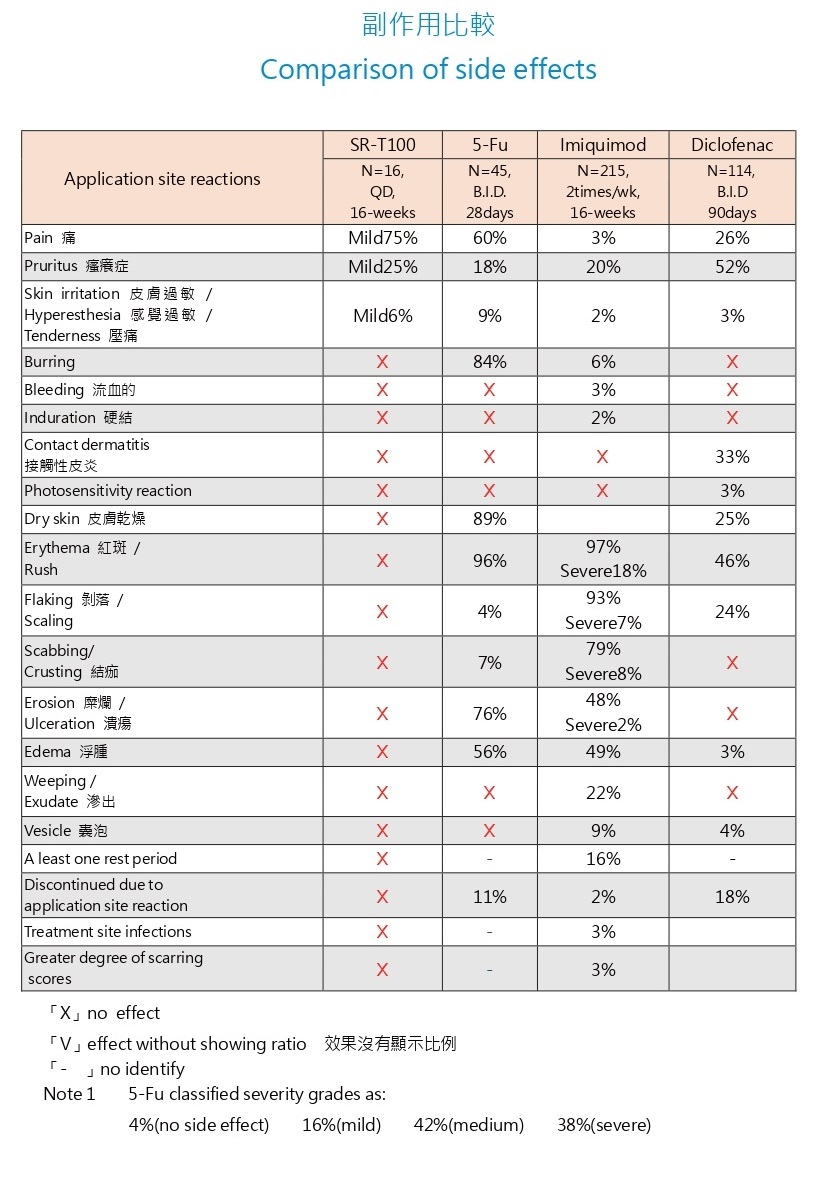
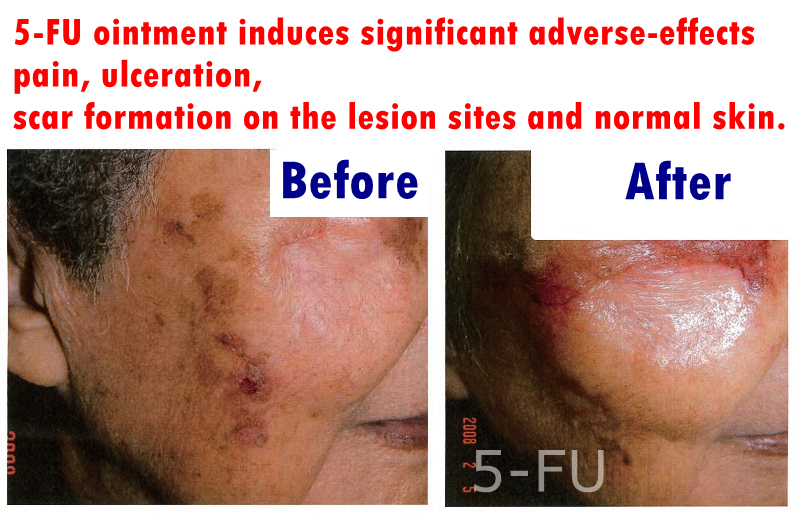
5-FU, 5% imiquimod cream, and 3% diclofenac gel are FDA-approved topical field therapies.
However, 5-FU ointment induces significant adverse-effects including pain, ulceration, and scar formation on the lesion sites and normal skin.
These side effects made 5-FU ointment an unpopular choice for treatment.
As for imiquimod cream and diclofenac gel, their low complete response rates, along with unfavorable side-effect profiles.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) involves applying a photosensitiser to the affected area prior to exposing it to a source of visible light.
Ingenol-mebutate gel
1. Ingenol-mebutate is a newer treatment for AK used in Europe and the United States.
2. First by disrupting cell membranes and mitochondria resulting cell death, and then by inducing antibody-dependent cellular cytotoxicity to eliminate remaining tumor cells.
3. Local skin reactions including pain, itching and redness can be expected during treatment with ingenol-mebutate.
Retinoids
Topical retinoids have been studied in the treatment of AK with modest results, and the American Academy of Dermatology does not currently recommend this as a first-line therapy.
The best treatment for actinic keratosis (Actinic keratoses / AK) 【Causes / Range / Symptoms / Types / Prevention / treatment】
Summary
1. The Solanum species herbs have been used to treat cancer for centuries
2. The efficacy and safety issues were addressed regarding topical treatment of Solamargine(SR-T100) on UVB-induced cutaneous SCC of hairless mice and actinic keratoses (AK) of human.
Results
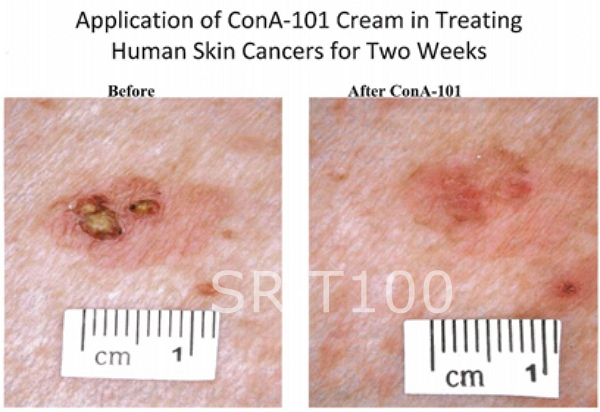
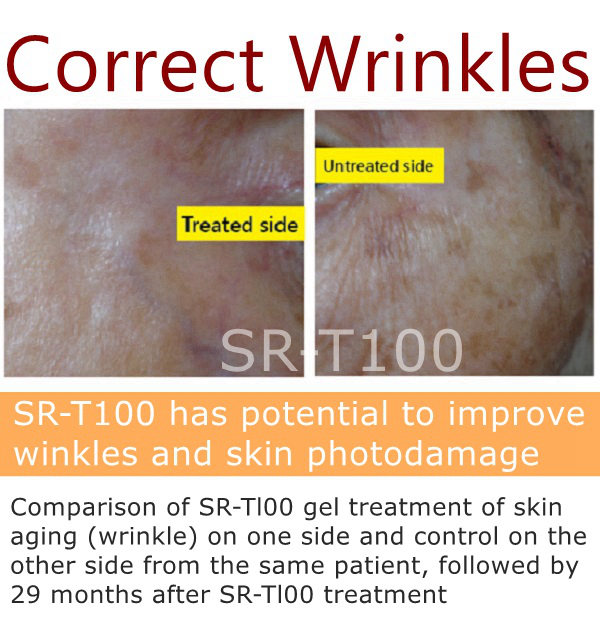
1. From our data, Solamargine(SR-T100) gel has shown a favorable profile for treating AK as compared to the aforementioned conventional topical therapies.
2. In terms of clinical response, Solamargine(SR-T100) showed an overall complete response rate of 70%.
3. In terms of side-effects, Solamargine(SR-T100) induced mild stinging and superficial erosions on the lesion sites and slight xerotic change on normal skin of both hairless mouse and human subjects after 10–16 weeks of topical use.
4. Taken together, topical Solamargine(SR-T100) may be an ideal candidate for treatment of AK due to its remarkable therapeutic efficacy on lesions and insignificant adverse effect on normal skin.


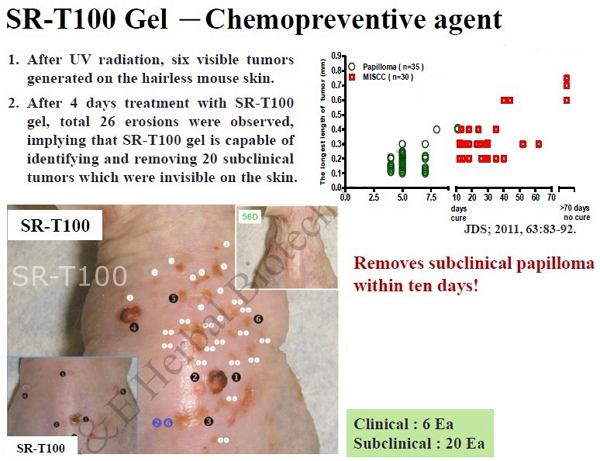
Solamargine(SR-T100) is best treatment for actinic keratosis (AK)
Condusions
Indication: actinic keratosis (AK)
Solamargine(SR-T100) is full compliance to FDA standard regulations of Chemistry, Manufacturing & Controls. 80% complete response rate observed with phase II clinical trial study.
The mechanism & active component identified by High Performance Liquid Chromatography methods(±10%) served as our scienfific basis in this technology.
Comparative study results showed Solamargine(SR-T100) has the least adverse effects among other similar products on the market (5-Fu, Imiquimod, Diclofenac & Ingenol Mebutate), complete elimination of actinic keratosis (AK) cells can be achieved in cryotherapy combination treatments, effectively prevents recurrence & suitable for treatment applications of actinic keratosis (AK) lesions in large skin surface areas.
Indication: common warts
Global patent registration in 2011 with preliminary data showing effective treatment against Verruca vulgaris (common warts), content ingredients found in marketed cosmetics product lines were proven effective in discharge of unsightly spots, skin bumps & blisters with very low adverse reactions.
This particular application has approved by FDA,
Indication: genital warts
Global patent registation in 2011 with concurrent trial study results (January 2011 to April 2013) showing a high complete response & has the least adverse side effects compared with its counterpart medications on the market. This application has approved by FDA.
From the data, Solamargine(SR-T100) gel has shown a favorable profile for treating AK as compared to the aforementioned conventional topical therapies.
In terms of clinical response, Solamargine(SR-T100) showed an overall complete response rate of 70%.
In terms of side-effects, Solamargine(SR-T100) induced mild stinging and superficial erosions on the lesion sites and slight xerotic change on normal skin of both hairless mouse and human subjects after 10–16 weeks of topical use.
Taken together, topical Solamargine(SR-T100) may be an ideal candidate for treatment of AK due to its remarkable therapeutic efficacy on lesions and insignificant adverse effect on normal skin.
Conclusions
1. Solamargine(SR-T100) is effective for the treatment of human vulva condyloma, with few side effects.
2. Compared with those with high-risk HPVs, cells with low-risk HPVs were more sensitive to Solamargine(SR-T100) treatment.
3. Autophagy played a protective role in Solamargine(SR-T100)-induced apoptosis in HPV-infected cells.
4. Our pilot study showed that Solamargine(SR-T100) was effective for the treatment of human vulva condyloma and was associated with few side effects.
5. Furthermore, we showed that cells expressing LR HPVs were more sensitive to Solamargine(SR-T100) treatment than those expressing HR HPVs.
Features:
• Prevention of UV skin damages
• Softening of skin keratinocytes
• Restores skin elastic property
• Botanically derived natural plant extraction
• No adverse skin reaction
• Patent rights protection in 32nations
• Preservative & Pigment free
USE: Apply several times per day, preferably covers with dermal dressing on film for the best absorption
USAGE : Patented ingredients for enhancing the repair of skin damage from environment and sunlight (as indicated in patents)
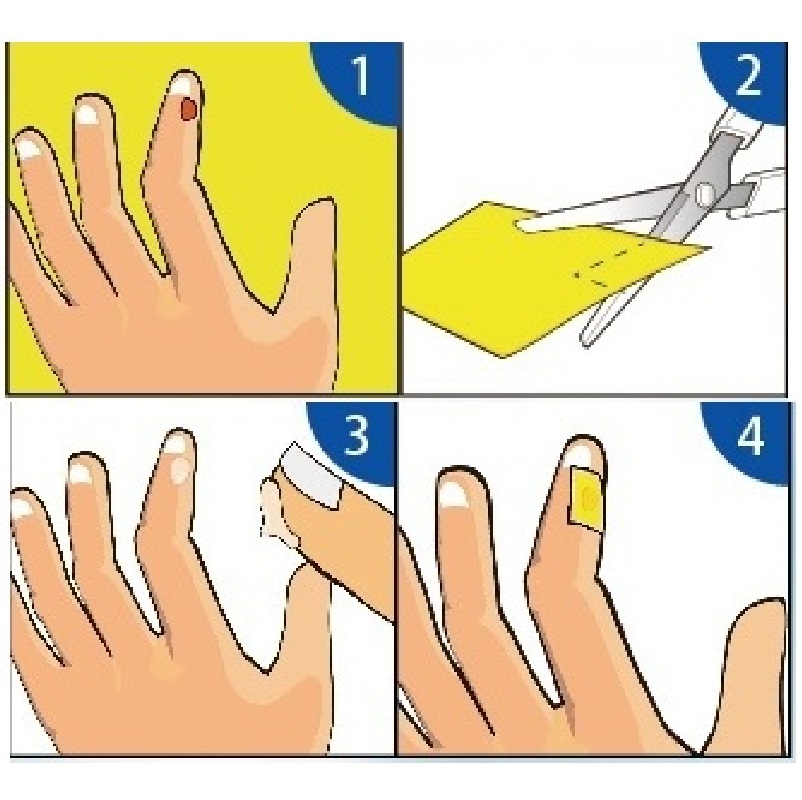
Instructions:
1. The cut artificial skin is large enough to completely cover the affected area.
2. Take an appropriate amount of ointment and apply it to the lesion.
3. Cover the cut artificial skin on the lesion.
TURBO Instructions:
1. In order to shorten the time course, the lesion can be treated with liquid nitrogen first, and then applied with ointment and then put a few artificial skins on the affected area.
2. If the artificial skin does not fall off, replace the ointment every two days. (Refill at any time depending on the situation)
The best treatment for actinic keratosis (Solar Keratoses / Actinic keratoses / AK)
The best treatments for warts (vulvar condyloma acuminatum, Genital warts)
The best treatment for squamous cell carcinoma (squamous cell cancer / SCC )
The best solution for cancer cells
Apoptotic (Correct/ Guide) bad behavior
Cure all diseases | Panacea | Package health
How to Longevity?
Want to Change?
Life Above All | Release life is best for oneself (me / yourself)
Eliminate misfortune!
Good affinities with others.
Beauty in Nature
Senile keratosis Contents
Senile keratosis Types
Senile keratosis Cause
Senile keratosis Pathophysiology
Senile keratosis Diagnosis
Senile keratosis Prevention
Senile keratosis Disinfection
Senile keratosis Treatment
Senile keratosis Medication
Senile keratosis Procedures
Senile keratosis Alternative medicine
Senile keratosis History
Senile keratosis Other animals
Senile keratosis References
Senile keratosis External links
0 Actinic Keratosis Contents
1 Epidemiology of actinic keratosis
2 Symptoms of actinic keratosis
3 Histopathological characteristics of actinic keratosis
4 List of differentiated diseases of actinic keratosis
5 Treatment of Actinic Keratosis
6 Prognosis of Actinic Keratosis
7 Footnotes to Actinic Keratosis
8 References for Actinic Keratosis
9 Actinic keratosis related items
Actinic keratosis is a skin lesion caused by long-term ultraviolet radiation.
Actinic keratosis is most common on the skin of the face, auricles, forearms, and back of hands that are susceptible to sunlight.
Unlike the so-called sunburn caused by acute sunlight exposure, DNA mutations will occur and develop after years of long-term UV exposure.
Although actinic keratosis is a precursor of skin cancer, only a few percent will actually develop into carcinoma in situ or invasive carcinoma.
Among solar ultraviolet rays, ultraviolet rays in the UV-B region (280-320nm) can cause DNA damage to epidermal cells.
In recent years, the relationship between the destruction of the stratospheric ozone layer, which has become an environmental issue, and skin cancer, has become more and more important.
Epidemiology of Actinic Keratosis
Most patients with actinic keratosis are middle-aged and elderly people.
There is no gender difference in actinic keratosis, but it is more common in men.
The prevalence of blacks and yellows is lower than that of whites.
People who are more likely to have erythema on their skin when sunburned are more likely to develop actinic keratosis than people who are brown.
Symptoms of Actinic Keratosis
Actinic keratosis has a flat, keratotic rash.
Actinic keratosis is a patchy lesion with a rough surface, usually a few millimeters to a maximum of 2 cm in size.
Actinic keratosis is reddish pink, brown or flesh-colored.
Actinic keratosis lesions usually occur on the face, around the auricles, back of the hands and forearms.
Actinic keratosis may be a single lesion, but there are also multiple lesions that occur at the same time or at different times.
In some cases, actinic keratosis may report mild itching, but subjective symptoms other than rash are rare.
Actinic keratosis is called the "corner of the skin" when it is severe.
Actinic keratosis lesions may resolve spontaneously, or they may recur in the same or different locations.
Precancerous lesions of actinic keratosis tend to resolve spontaneously, but in fact lesions that develop into squamous cell carcinoma are rare.
Actinic keratosis is a common skin lesion in the elderly.
However, actinic keratosis is a disease that should be checked regularly by a dermatologist.